Who is a Suitable Candidate for Implantable Collamer Lens?
Implantable Collamer Lens (ICL) is a revolutionary vision correction solution that has transformed the lives of many individuals worldwide. This article aims to provide comprehensive information about ICL, including its procedure, the ideal candidate profile, the associated risks and benefits, and post-procedure expectations. Whether you’re considering ICL for yourself or a loved one, this article is a valuable resource.
Understanding Implantable Collamer Lens
The Implantable Collamer Lens, or ICL, is a cutting-edge solution for correcting refractive errors such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. This innovative approach is gaining traction due to its reversible nature and the continuous advancements in the field. Unlike many vision correction methods, ICL does not permanently modify the structure of your eye. The procedure is as straightforward as wearing contact lenses, yet the results are enduring. This article will provide an in-depth understanding of the Implantable Collamer Lens and help you determine if you are a candidate for this vision correction procedure.
What is an Implantable Collamer Lens?
The Implantable Collamer Lens (ICL) is a state-of-the-art, biocompatible lens that is surgically placed into the eye to rectify refractive errors. The ICL is crafted from a unique substance called Collamer, a collagen-based material that harmonizes with the eye’s natural environment, allowing the lens to remain in place indefinitely.
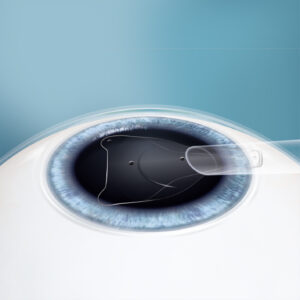
Positioned behind the iris and in front of the eye’s natural lens, the ICL sharpens focus and corrects vision errors without the need to remove or permanently alter any corneal tissue. This makes it an attractive option for patients who are not candidates for LASIK or PRK surgeries or for those who prefer a removable vision correction solution. The ICL can be replaced or removed if the eye’s prescription changes, offering the advantage of reversibility.
The ICL procedure is typically swift, often completed within 20-30 minutes, and can correct a broader range of vision errors compared to other methods. The treatment is designed to provide a long-lasting solution, yet it retains the flexibility of being reversible if necessary. It is a personalized procedure tailored to each patient’s unique eye structure and visual requirements.
One of the key advantages of ICL is that it does not require the removal of corneal tissue, unlike other vision correction procedures. This makes it particularly beneficial for patients with thin corneas or high levels of refractive error. ICL broadens the scope of refractive surgery, making vision correction accessible to a wider population.
In the following sections, we will delve into the specifics of who is an ideal candidate for ICL, the procedure itself, potential risks and benefits, and what to expect after the procedure.
Procedure for ICL Implantation
The journey to clearer vision through an Implantable Collamer Lens (ICL) begins with a straightforward outpatient procedure. Typically, each eye requires around 20 to 30 minutes of surgical time. Let’s look at the step-by-step process:
Preparation: The journey begins with a thorough examination by the ophthalmologist. They will measure the shape and size of your eye to ensure the ICL fits perfectly. It’s important to refrain from wearing contact lenses for a specified period before these measurements.
Anesthesia: On the day of the surgery, your eye is numbed using topical anesthesia drops. This ensures minimal discomfort during the procedure. Sometimes, a mild sedative may be administered to help you relax.
ICL Insertion: The surgeon makes a small incision in the cornea, through which the ICL lens is inserted. The collamer lens’s flexibility allows it to be folded and inserted through this tiny incision.
Positioning the ICL: The ICL is then carefully unfolded and positioned behind the iris and in front of the natural lens. Once in place, the ICL starts working immediately, similar to a contact lens.
Post-procedure: After the surgery, you’ll be prescribed antibiotics and anti-inflammation eye drops to aid in healing. As the procedure is minimally invasive, stitches are typically unnecessary, and the incision heals naturally over time.
A follow-up appointment is typically scheduled within 24 hours of surgery, and regular check-ups are recommended to ensure your eyes remain healthy.
Who is a Suitable Candidate for ICL?
The decision to opt for Implantable Collamer Lens (ICL) is not a one-size-fits-all solution. Several factors come into play when determining if you’re a suitable candidate for ICL. These include age, eyesight prescription, overall eye health, and lifestyle considerations. These elements ensure the lens fits properly and that the procedure will yield the desired results.
However, it’s important to understand that while ICL can be a fantastic solution for vision correction, it’s not suitable for everyone. A thorough evaluation and consultation with a qualified ophthalmologist are essential to determine if ICL is the right choice for you. In the subsequent sections, we’ll look deeper into the specific requirements, such as age, eyesight, and health considerations that make a person suitable for ICL.
Age and Eyesight Requirements for ICL
When evaluating a potential candidate for ICL, age, and vision stability are two fundamental aspects.
Age: The ideal age bracket for ICL candidates typically falls between 21 and 45 years. This is primarily because refractive errors are most likely to have settled during this period. The individual’s vision prescription must be stable for at least a year before the procedure. For those under 21, their vision may still be changing significantly, and for those over 45, other procedures such as refractive lens exchange or mono vision LASIK might be more beneficial due to the onset of presbyopia.
Vision Prescription: ICL can effectively address a broad spectrum of refractive errors. It is especially advantageous for those with moderate to high myopia (nearsightedness), typically between -3.00D to -15D, and reduces nearsightedness up to -20.00 diopters. It can also rectify astigmatism up to 4.00 diopters. However, it’s important to understand that the exact correction range can vary based on individual eye anatomy.
Individuals aged between 21 and 45 with a stable vision prescription within the specified ranges would be an ideal candidate for ICL. However, these are general guidelines and a comprehensive eye examination by a qualified ophthalmologist is necessary to determine the appropriateness of the procedure for each patient.
Health Considerations for ICL Candidates
In addition to age and vision prescription, the eye’s overall health significantly determines ICL candidacy. Here are some key health factors that are considered:
Eye Health: ICL candidates should ideally have healthy eyes with no glaucoma, iritis, or corneal abnormalities history. A healthy endothelial cell count (cells lining the back of the cornea) is vital as these cells help maintain corneal clarity. Any condition that compromises these cells could potentially disqualify a candidate for ICL.
Anterior Chamber Depth: The depth of the eye’s front chamber is another factor. There must be sufficient space in the anterior chamber to accommodate the lens. Typically, the anterior chamber depth should be greater than 3.00mm.
Pupil Size: Pupil size is also considered as larger pupils may increase the likelihood of post-procedure glare and halos.
Pregnancy or Nursing: Women who are pregnant or nursing may need to defer the procedure until their hormones have stabilized, as these changes can impact vision stability.
Moreover, good health is generally required as conditions like diabetes or autoimmune disorders can affect post-surgery healing.
Even if patients don’t meet all these criteria, they may still be eligible for ICL. Each patient’s situation is unique, and a comprehensive evaluation with an experienced surgeon is the best way to ascertain if ICL is the right choice.
Understanding the Risks and Benefits of ICL
Embarking on the vision correction journey through Implantable Collamer Lens (ICL) implantation requires a comprehensive understanding of the potential benefits and risks involved. This knowledge is pivotal in making an informed decision about your eye health. In this section, we will explore the various advantages of ICL and shed light on the potential risks and complications accompanying this procedure. This will underscore the importance of the candidate suitability criteria discussed earlier. You can make a more informed decision about your vision correction path by grasping the full pros and cons.
Benefits of Choosing ICL
Opting for an Implantable Collamer Lens as a vision correction method brings many benefits, contributing to its increasing preference among various vision correction alternatives. Let’s delve into what makes ICL an attractive option:
Superior Vision Quality: ICL often yields a superior quality of vision, enhancing depth and dimension perception. Many patients have reported a noticeable enhancement in their vision clarity, rendering it more precise and vivid.
Extensive Correction Scope: As mentioned earlier, ICL can correct a broad spectrum of refractive errors. This includes higher degrees of myopia that may not qualify for other vision correction procedures.
Corneal Structure Preservation: Unlike laser procedures that necessitate corneal reshaping, ICLs are inserted inside the eye, thereby preserving the corneal structure. This is particularly beneficial for patients with thin corneas.
Reversibility: If a patient is dissatisfied with the vision post-ICL implantation or if there are significant changes to vision prescriptions later in life, the ICL can be removed or replaced.
Rapid Recovery: Typically, patients witness a swift recovery and can observe an improvement in vision as early as the day following surgery.
UV Protection: The Collamer material used in ICL provides protection from the sun’s harmful UV rays, offering an added benefit alongside vision correction.
While these advantages are compelling, remember that the ultimate decision to proceed with ICL should be made after a thorough eye examination and consultation with an experienced ophthalmologist to balance these benefits against any potential risks.
Recognizing the Risks and Potential Complications of ICL
While the ICL procedure is generally safe and effective, like any surgical intervention, it carries a certain degree of risk. It is essential to be aware of these potential complications, even though they are relatively rare. Here are some of the risks associated with ICL:
Infection: Infections can occur during or after any surgical procedure, including ICL. However, with proper pre- and post-operative care, this risk can be significantly reduced.
Cataracts: A small percentage of patients may develop cataracts post-procedure. This condition occurs when the lens inside the eye, located behind the ICL, clouds over. An experienced surgeon can manage this risk by carefully selecting the correct ICL size and employing meticulous surgical techniques.
Glaucoma: In a few cases, ICL may cause an increase in eye pressure, potentially leading to glaucoma. Regular eye pressure monitoring post-surgery is crucial to prevent this.
Visual Disturbances: Some patients may experience halos, glare, or double vision, especially in low light or at night. Factors like pupil size and ICL position can contribute to these symptoms.
ICL Displacement: On rare occasions, the ICL may shift from its intended position, requiring a minor procedure to correct its placement.
Despite these potential complications, it’s important to remember that the incidence of complications in ICL surgery is quite low, thanks to modern surgical techniques and technology. Regular check-ups and diligent eye care can further minimize these risks. Discussing these potential risks with your ophthalmologist to make an informed decision about ICL is always advisable.
Post-Procedure Expectations for ICL Patients
Understanding what to expect after the ICL procedure is crucial to knowing the candidacy factors, risks, and benefits. This knowledge spans from the immediate recovery period following the surgery to the long-term outcomes of ICL implantation. It’s important to note that each patient’s recovery process and long-term results may vary based on their unique health conditions and specific vision correction needs. Maintaining open communication with your eye care professional can facilitate a smoother recovery journey and prepare you for the transformative benefits that ICL can offer in the long term.
Understanding the Recovery Period
Navigating the recovery period post-ICL surgery is part of the process. Let’s look into what you can anticipate:
Immediately After Surgery: A mild discomfort may be experienced in your eyes following the procedure. This is a temporary sensation, expected to subside within a few hours. Your surgeon may provide a protective shield to protect your eyes from accidental rubbing or pressure.
The Day Following Surgery: A significant improvement in vision is typically noticed by most patients within the first 24 hours after surgery. Daily activities can usually be resumed at this point. A post-operative check-up will be scheduled to ensure your eyes heal as expected.
The First Week: Mild irritation, light sensitivity, or minor discomfort may be experienced during the initial week. Refrain from rubbing your eyes during this period to promote healing.
Medication: Your doctor may prescribe eye drops containing antibiotics and anti-inflammatory medications to aid in the healing process and manage discomfort. Adherence to the prescribed regimen is essential.
Extended Recovery: Over the weeks following the ICL procedure, your vision should stabilize, and minor complications such as halos or glares should diminish. Regular follow-up appointments with your eye care provider are important during this period.
Remember, healing is a personal process and varies from person to person. Adhering to your doctor’s advice is the key to a successful recovery following ICL surgery.
Long-Term Outcomes of ICL
The decision to undergo ICL surgery extends beyond the recovery period. It’s about the enduring benefits and outcomes it brings to your vision. Here’s what you can expect long-term:
Consistent Vision Improvement: Post-recovery, patients often report a stable, high-quality vision, which can be as good as 20/20 or even better. This significant improvement often reduces or eliminates the need for corrective eyewear.
Adaptability: ICL offers the unique advantage of being reversible. If your prescription changes significantly over time, the implanted lens can be replaced to match the new prescription, ensuring optimal vision throughout your life.
Effectiveness Over Time: ICLs are designed to offer permanent vision correction. However, changes in vision due to the natural aging process can still occur. Regular follow-ups with your eye care provider will help maintain your vision at its best.
Post-ICL surgery, patients often find they can engage more fully in activities without the inconvenience of glasses or contact lenses, enhancing their quality of life. Regular eye check-ups and proper eye care remain essential for maintaining optimal eye health. Remember that these long-term outcomes can vary based on individual health conditions and lifestyle. It’s always recommended to discuss your personal expectations with your ophthalmologist.
1. What defines a suitable candidate for Implantable Collamer Lens (ICL)?
An ideal candidate for Implantable Collamer Lens (ICL) is usually someone aged between 21 and 45, with a stable prescription and myopia between -3D and -20D. Patients should not have any eye infections or diseases.
2. Is there an age limit for becoming a suitable ICL candidate?
Persons aged between 21 and 45 are usually considered ideal candidates for an ICL procedure. However, older individuals aren’t automatically disqualified; decisions are decided case by case, considering overall eye health and vision requirements. Speak with an experienced ophthalmologist.
3. How can a person’s prescription determine their suitability for an Implantable Collamer Lens procedure?
A stable prescription, meaning the eyesight prescription has not changed significantly in the past year, is a key factor in determining ICL candidacy. Excessive myopia or hypermetropia can, however, disqualify a candidate.
4. Can pre-existing eye conditions affect candidacy for an ICL procedure?
Yes. Pre-existing eye diseases such as glaucoma, cataracts, or previous eye surgeries can impact candidacy for an ICL procedure. Eye health and clarity should be optimal for the procedure’s success.
5. Are people who have undergone previous eye surgeries eligible for ICL?
Previous ocular surgeries could potentially disqualify a candidate from an ICL procedure. The suitability of these candidates must be assessed on a case-by-case basis, considering the type and success of previous surgeries.
6. Does general health condition factor into becoming an ICL candidate?
While the focus is primarily on the eyes’ health, good general health is also vital for any surgery, including an ICL procedure. Hence, any serious health conditions could inevitably impact the decision.
Sources:
https://www.accessdata.fda.gov/cdrh_docs/pdf3/P030016S035D.pdf