Intraoperative Aberrometry for Cataract Patients with Post-Refractive Surgery (after LASIK)

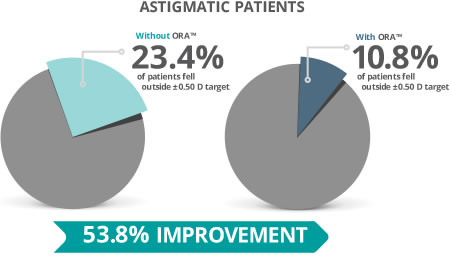
ORA measures your prescription during cataract surgery after the cataract has been removed. If you have had laser vision correction (LASIK, PRK or RK) you would benefit from the use of ORA. During any laser vision correction surgery, the cornea is manipulated and that can alter some of the measurements we get during your pre-op exam. The use of ORA also helps identify the level of astigmatism you have in the back of your eye. So, if you have astigmatism, ORA will measure your eye and correctly identify the level of power you need in your lens at the time of surgery.
Please read the following data as it shows studies from several different sources on why ORA is beneficial to patients.
For the past couple of decades, there has been a significant amount of research on increasing the accuracy and precision of the intraocular lens (IOL) selection in cataract surgery. For effective refractive outcomes, accuracy in optical biometry is crucial.
In a sea of the latest high tech tools used in ophthalmic surgery, some believe that intraoperative aberrometry ORA may help cataract surgeons in the lens selection of post LASIK surgery patients.
Intraoperative aberrometry aims to minimize residual refractive error via aphakic refraction, allowing cataract surgeons to revise or confirm the IOL selection achieved through preoperative biometry, as well as improve lens location and customize arcuate corneal incisions, according to an eye’s astigmatic requirements.
Intraoperative Aberrometry Backstory
Intraoperative aberrometry is the recent successor of a portable, handheld device created by Tsontcho “Sean” Ianchulev, MD, MPH at the Doheny Eye Institute. The device was designed to develop a tool that did not need keratometry measurements and axial lengths to provide accurate refraction.
The ORange wavefront aberrometry system was ORA’s latest forerunner, which was replaced by ORA later on.
ORA is mounted on an operating microscope and uses infrared light and Talbot-Moiré interferometry, amplified for the aphakic state of -5 to+20 D, to perform a complete eye assessment of the refractive power of the optical system. ORA takes 40 measurements within less than a minute.
The system shows the scans in order, combines data and analyzes it from the central 4mm to decide the best IOL power for the eye.
Research in Post-Refractive Surgery
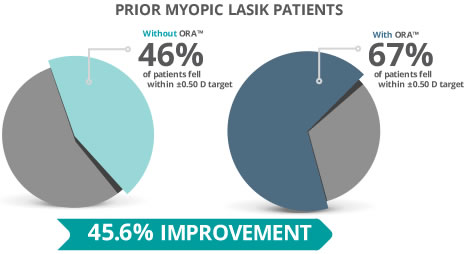
Eyes that have undergone refractive surgery and LASIK pose a challenge to surgeons making IOL selection. Studies report that less than 55% of post-LASIK eyes following cataract surgery showed ±0.5D of emmetropia, versus 70% in eyes that hadn’t undergone prior refractive surgery.
Earlier studies that used ORange technology in eyes that received prior myopic correcting treatment indicated that only 39% of the eyes were within ±0.5D of emmetropia, whereas 60% were within ±1D.
However, more recent studies that use ORA technology show more promising results in this subset. One study showed that ORA had the highest predictive accuracy of IOL power compared to Shammas formula, Haigis L formula and a combination of clinical data of the surgeon’s choice.
With ORA, researchers found a medium absolute error of 0.35D compared to 0.51 with Shammas, 0.53 with Haigis and 0.6 of surgeon’s choice. 67% fell within ±0.5 D and 94%, within ±15.
Another study comparing 0RA to the Fourier-domain OCT based formula, Masket regression formula and Haigas-L formula, showed a 0.25 D median absolute error for ORA.
Benefits of Intraoperative Aberrometry
Cataract surgery planning comes with its own set of uncertainties. Doctors believe it helps by minimizing some of the following issues:
- ORA reduces guesswork Up until recently, doctors had to make their best guess built on preoperative biometry, regarding marking the cornea prior to surgery, what the optimum lens strength should be to implant, the most effective axis for a toric lens and so on.ORA allows doctors to continue rotating the IOL until the aberrometer indicates that they’ve reduced astigmatism. Alternatively, doctors can exchange the lens, in case the power isn’t accurate. Intraoperative aberrometry allows doctors to deliver optimum refractive outcomes in a simple, convenient and noninvasive way, without making changes to their surgical routines. ORA allows doctors to reduce average errors of more than 0.75D (and even 1 and 2 D) significantly, without breaking the bank.
- ORA identifies posterior astigmatism Aphakic refraction takes factors, such as posterior corneal astigmatism, into account, indicating that ORA is a useful system in detecting posterior astigmatism. When not identified by traditional biometry, refractive errors as a result of unnoticed posterior astigmatism can come by surprise post cataract surgery. According to a study led by Koch and colleagues, which included 715 eyes in 435 patients, the average posterior corneal astigmatism was -0.3D. Researchers concluded that selecting a toric IOL power, based only on anterior surface measurements could lead to the following outcomes:
- Cause a total astigmatism error by 0.22 at the 180 meridian. And underestimate total astigmatism by 0.50 D in 5% of eyes.
- Eyes with with-the-rule astigmatism may have toric overcorrection
- Eyes with against-the-rule astigmatism may experience under-correction of the eyes
- ORA helps manage astigmatism correcting incisions As laser-assisted surgery becomes more common in the medical industry, one other area where ORA is particularly useful is in managing astigmatism correcting incisions.
Once the IOL has been inserted and the eye is pressurized, the refractive data from the system can indicate how much residual astigmatism is present, helping doctors determine if incisions are required to be extended or opened. - ORA benefits patients Patients who are paying more for toric or presbyopic IOLS could particularly benefit from the predictability of refractive outcomes. Furthermore, patients who have undergone LASIK or PRK, often have higher expectations in their visual results because this has already been proven by them choosing to go through refractive surgery (LASIK). In most cases, their reshaped corneas can hinder conventional biometry and ORA can assist in increased refractive outcomes.
- ORA requires fewer enhancements According to a survey conducted by Shareef Mahdavi, ophthalmologists who frequently use the device stated that their enhancement rates dropped by about half, from an average of 10 percent to 5.3 percent.
Surgical Considerations
To obtain accurate results from this revolutionary new technology, users are required to pay closer attention to details. For example, while testing aphakic refraction, the incision made has to be sealed without being over-hydrated, IOP must be set to physiologic levels as measured using a tonometer, the central cornea must be kept clear, among other details.
In addition, the surgeon should also ensure that there is no eye tilt while measurements are being taken.
Ultimately, surgeons agree that although these steps add time, they also add a premium feature to cataract surgery. ORA and similar tools are designed for surgeons who are particular about results.
As technologies advance, patient expectations rise as well. This makes ORA a vital tool in cataract surgery.
LaserCare Eye Center has extensive experience performing cataract surgery in patients with a history of LASIK Surgery. We use both ORA and the Lensx laser for cataract surgery.